Aspectos relevantes de la enfermedad por hígado graso no alcohólico
DOI:
https://doi.org/10.52784/27112330.137Palabras clave:
enfermedad del hígado graso no alcohólico, hígado graso, cirrosis hepática, carcinoma hepatocelular.Resumen
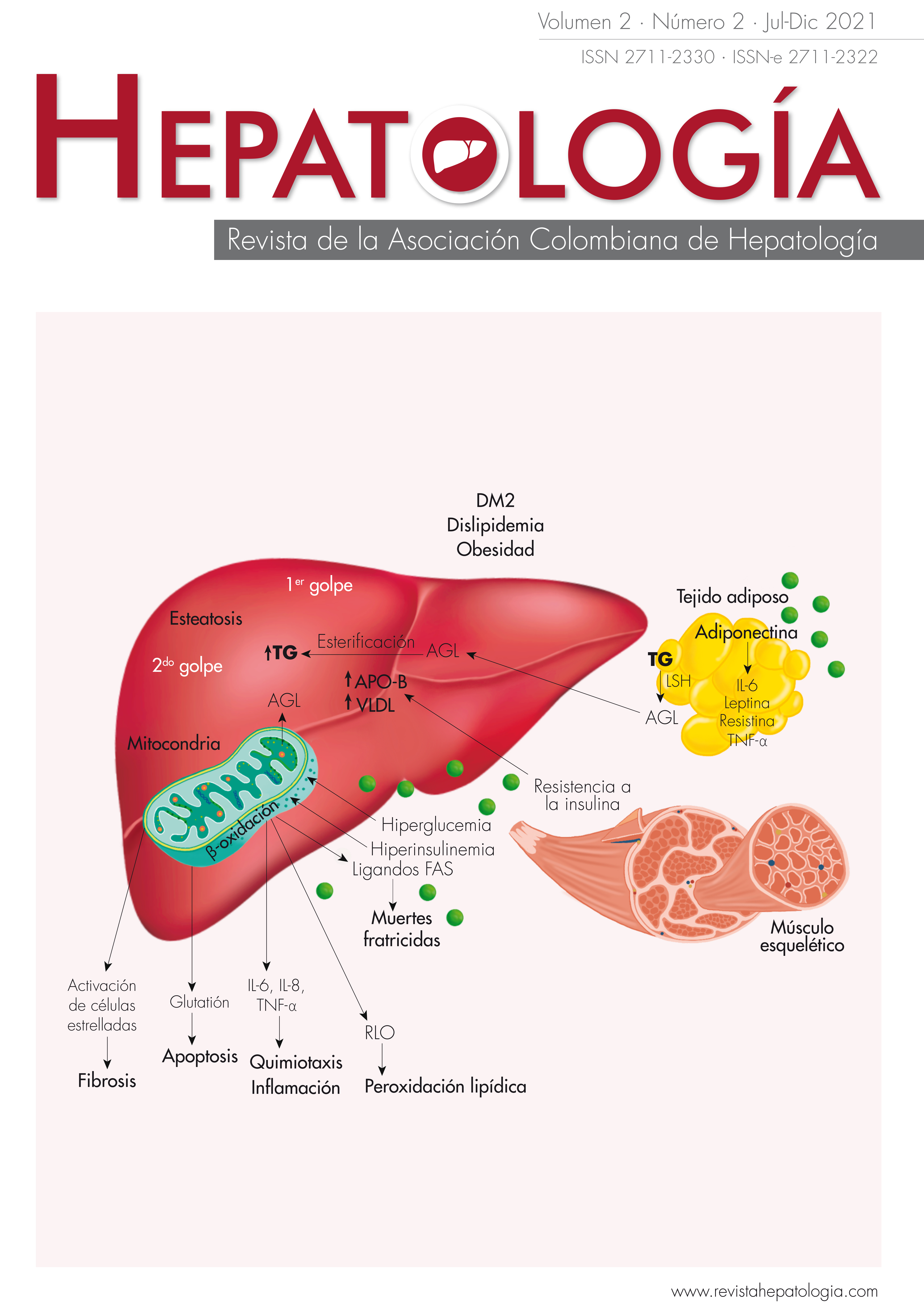
La enfermedad por hígado graso no alcohólico (EHGNA) es una condición que incluye desde la esteatosis hepática simple y la esteatohepatitis, hasta la cirrosis hepática y eventualmente el carcinoma hepatocelular. La diabetes tipo 2 y la obesidad son los principales factores asociados a la EHGNA. Su prevalencia en la población general se ha descrito entre el 20% y el 30%. Estos pacientes tienen un riesgo aumentado de mortalidad y presentan mayor incidencia que la población general de complicaciones hepáticas y cardiovasculares. La asociación de diferentes factores promueve la acumulación de ácidos grasos en el parénquima hepático, generando un estado de estrés, con formación de radicales de oxígeno y liberación de citoquinas inflamatorias que determinan la progresión de la enfermedad. Aunque existen diferentes pruebas no invasivas para el diagnóstico y estadificación de esta entidad, la biopsia hepática es la única prueba que permite identificar de manera fiable la presencia de inflamación, además del grado de fibrosis. El tratamiento actual de la EHGNA se basa en los cambios de estilo de vida del paciente, que han demostrado ser efectivos, incluso para revertir la fibrosis. Desafortunadamente, la adherencia a las medidas generales es muy pobre, de ahí la necesidad de contar con estrategias farmacológicas. Hasta el momento, no contamos con medicamentos aprobados por las agencias regulatorias para esta entidad, y los únicos fármacos recomendados por las sociedades internacionales son la pioglitazona y la vitamina E, que no están exentas de efectos adversos. Actualmente se encuentran bajo investigación diferentes medicamentos que buscan reducir la actividad inflamatoria sin aumento de la fibrosis, o mejoría de la fibrosis sin deterioro de la esteatohepatitis.
Descargas
Referencias bibliográficas
Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology 1999;116:1413-1419. https://doi.org/10.1016/s0016-5085(99)70506-8.
Caldwell SH, Oelsner DH, Iezzoni JC, Hespenheide EE, Battle EH, Driscoll CJ. Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease. Hepatology 1999;29:664-669. https://doi.org/10.1002/hep.510290347.
Bellentani S, Scaglioni F, Marino M, Bedogni G. Epidemiology of non-alcoholic fatty liver disease. Dig Dis 2010;28:155-161. https://doi.org/10.1159/000282080.
Younossi ZM, Otgonsuren M, Henry L, Venkatesan C, Mishra A, Erario M, et al. Association of nonalcoholic fatty liver disease (NAFLD) with hepatocellular carcinoma (HCC) in the United States from 2004 to 2009. Hepatology 2015;62:1723-1730. https://doi.org/10.1002/hep.28123.
Younes R, Bugianesi E. Should we undertake surveillance for HCC in patients with NAFLD? J Hepatol 2018;68:326-334. https://doi.org/10.1016/j.jhep.2017.10.006.
Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology 2005;129:113-121. https://doi.org/10.1053/j.gastro.2005.04.014.
Piscaglia F, Svegliati-Baroni G, Barchetti A, Pecorelli A, Marinelli S, Tiribelli C, et al. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: A multicenter prospective study. Hepatology 2016;63:827-838. https://doi.org/10.1002/hep.28368.
Younossi ZM, Stepanova M, Afendy M, Fang Y, Younossi Y, Mir H, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol 2011;9:524-530.e521; quiz e560. https://doi.org/10.1016/j.cgh.2011.03.020.
Falck-Ytter Y, Younossi ZM, Marchesini G, McCullough AJ. Clinical features and natural history of nonalcoholic steatosis syndromes. Semin Liver Dis 2001;21:17-26. https://doi.org/10.1055/s-2001-12926.
Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc 1980;55:434-438.
Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology 2011;140:124-131. https://doi.org/10.1053/j.gastro.2010.09.038.
Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology 2004;40:1387-1395. https://doi.org/10.1002/hep.20466.
Daly AK, Ballestri S, Carulli L, Loria P, Day CP. Genetic determinants of susceptibility and severity in nonalcoholic fatty liver disease. Expert Rev Gastroenterol Hepatol 2011;5:253-263. https://doi.org/10.1586/egh.11.18.
Medina J, Fernández-Salazar LI, García-Buey L, Moreno-Otero R. Approach to the pathogenesis and treatment of nonalcoholic steatohepatitis. Diabetes Care 2004;27:2057-2066. https://doi.org/10.2337/diacare.27.8.2057.
Targher G, Marra F, Marchesini G. Increased risk of cardiovascular disease in non-alcoholic fatty liver disease: causal effect or epiphenomenon? Diabetologia 2008;51:1947-1953. https://doi.org/10.1007/s00125-008-1135-4.
Solís Herruzo JA, García Ruiz I, Pérez Carreras M, Muñoz Yagüe MT. Non-alcoholic fatty liver disease. From insulin resistance to mitochondrial dysfunction. Rev Esp Enferm Dig 2006;98:844-874. https://doi.org/10.4321/s1130-01082006001100006.
Day CP, James OF. Steatohepatitis: a tale of two "hits"? Gastroenterology 1998;114:842-845. https://doi.org/10.1016/s0016-5085(98)70599-2.
Medina J, Moreno-Otero R. Pathophysiological basis for antioxidant therapy in chronic liver disease. Drugs 2005;65:2445-2461. https://doi.org/10.2165/00003495-200565170-00003.
Sanz-Cameno P, Medina J, García-Buey L, García-Sánchez A, Borque MJ, Martín-Vílchez S, et al. Enhanced intrahepatic inducible nitric oxide synthase expression and nitrotyrosine accumulation in primary biliary cirrhosis and autoimmune hepatitis. J Hepatol 2002;37:723-729. https://doi.org/10.1016/s0168-8278(02)00266-0.
García-Monzón C, Martín-Pérez E, Iacono OL, Fernández-Bermejo M, Majano PL, Apolinario A, et al. Characterization of pathogenic and prognostic factors of nonalcoholic steatohepatitis associated with obesity. J Hepatol 2000;33:716-724. https://doi.org/10.1016/s0168-8278(00)80301-3.
Mallat A, Lotersztajn S. Endocannabinoids and liver disease. I. Endocannabinoids and their receptors in the liver. Am J Physiol Gastrointest Liver Physiol 2008;294:G9-12. https://doi.org/10.1152/ajpgi.00467.2007.
Petersen KF, Dufour S, Hariri A, Nelson-Williams C, Foo JN, Zhang XM, et al. Apolipoprotein C3 gene variants in nonalcoholic fatty liver disease. N Engl J Med 2010;362:1082-1089. https://doi.org/10.1056/NEJMoa0907295.
Kral JG, Lundholm K, Björntorp P, Sjöström L, Scherstén T. Hepatic lipid metabolism in severe human obesity. Metabolism 1977;26:1025-1031. https://doi.org/10.1016/0026-0495(77)90020-8.
Sanyal AJ, Campbell-Sargent C, Mirshahi F, Rizzo WB, Contos MJ, Sterling RK, et al. Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology 2001;120:1183-1192. https://doi.org/10.1053/gast.2001.23256.
Ferrannini E, Barrett EJ, Bevilacqua S, DeFronzo RA. Effect of fatty acids on glucose production and utilization in man. J Clin Invest 1983;72:1737-1747. https://doi.org/10.1172/jci111133.
Sastre J, Pallardó FV, Llopis J, Furukawa T, Viña JR, Viña J. Glutathione depletion by hyperphagia-induced obesity. Life Sci 1989;45:183-187. https://doi.org/10.1016/0024-3205(89)90293-2.
Strauss RS, Barlow SE, Dietz WH. Prevalence of abnormal serum aminotransferase values in overweight and obese adolescents. J Pediatr 2000;136:727-733.
Baskol G, Baskol M, Kocer D. Oxidative stress and antioxidant defenses in serum of patients with non-alcoholic steatohepatitis. Clin Biochem 2007;40:776-780. https://doi.org/10.1016/j.clinbiochem.2007.02.006.
Yu J, Chu ES, Wang R, Wang S, Wu CW, Wong VW, et al. Heme oxygenase-1 protects against steatohepatitis in both cultured hepatocytes and mice. Gastroenterology 2010;138:694-704. https://doi.org/10.1053/j.gastro.2009.09.058.
Viganò M, Vergani A, Trombini P, Paleari F, Piperno A. Insulin resistance influence iron metabolism and hepatic steatosis in type II diabetes. Gastroenterology 2000;118:986-987. https://doi.org/10.1016/s0016-5085(00)70193-4.
Asilmaz E, Cohen P, Miyazaki M, Dobrzyn P, Ueki K, Fayzikhodjaeva G, et al. Site and mechanism of leptin action in a rodent form of congenital lipodystrophy. J Clin Invest 2004;113:414-424. https://doi.org/10.1172/JCI19511.
Xu A, Wang Y, Keshaw H, Xu LY, Lam KS, Cooper GJ. The fat-derived hormone adiponectin alleviates alcoholic and nonalcoholic fatty liver diseases in mice. J Clin Invest 2003;112:91-100. https://doi.org/10.1172/jci17797.
Savvidou S, Hytiroglou P, Orfanou-Koumerkeridou H, Panderis A, Frantzoulis P, Goulis J. Low serum adiponectin levels are predictive of advanced hepatic fibrosis in patients with NAFLD. J Clin Gastroenterol 2009;43:765-772. https://doi.org/10.1097/MCG.0b013e31819e9048.
Ilan Y. Leaky gut and the liver: a role for bacterial translocation in nonalcoholic steatohepatitis. World J Gastroenterol 2012;18:2609-2618. https://doi.org/10.3748/wjg.v18.i21.2609.
European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD), European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016;64:1388-1402. https://doi.org/10.1016/j.jhep.2015.11.004.
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018;67:328-357. https://doi.org/10.1002/hep.29367.
Sheth SG, Gordon FD, Chopra S. Nonalcoholic steatohepatitis. Ann Intern Med 1997;126:137-145. https://doi.org/10.7326/0003-4819-126-2-199701150-00008.
Fierbinteanu-Braticevici C, Dina I, Petrisor A, Tribus L, Negreanu L, Carstoiu C. Noninvasive investigations for non alcoholic fatty liver disease and liver fibrosis. World J Gastroenterol 2010;16:4784-4791. https://doi.org/10.3748/wjg.v16.i38.4784.
European Association for Study of Liver, Asociacion Latinoamericana para el Estudio del Hígado. EASL-ALEH Clinical Practice Guidelines: Non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol 2015;63:237-264. https://doi.org/10.1016/j.jhep.2015.04.006.
Guha IN, Parkes J, Roderick P, Chattopadhyay D, Cross R, Harris S, et al. Noninvasive markers of fibrosis in nonalcoholic fatty liver disease: Validating the European Liver Fibrosis Panel and exploring simple markers. Hepatology 2008;47:455-460. https://doi.org/10.1002/hep.21984.
McPherson S, Anstee QM, Henderson E, Day CP, Burt AD. Are simple noninvasive scoring systems for fibrosis reliable in patients with NAFLD and normal ALT levels? Eur J Gastroenterol Hepatol 2013;25:652-658. https://doi.org/10.1097/MEG.0b013e32835d72cf.
Wong VW, Vergniol J, Wong GL, Foucher J, Chan HL, Le Bail B, et al. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease. Hepatology 2010;51:454-462. https://doi.org/10.1002/hep.23312.
Petta S, Vanni E, Bugianesi E, Di Marco V, Cammà C, Cabibi D, et al. The combination of liver stiffness measurement and NAFLD fibrosis score improves the noninvasive diagnostic accuracy for severe liver fibrosis in patients with nonalcoholic fatty liver disease. Liver Int 2015;35:1566-1573. https://doi.org/10.1111/liv.12584.
Romero FP. Will non-invasive testing replace liver biopsy in the diagnosis and follow-up of non-alcoholic steatohepatitis (NASH)? Rev Esp Enferm Dig 2009;101:521-527. https://doi.org/10.4321/s1130-01082009000800001.
Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol 1999;94:2467-2474. https://doi.org/10.1111/j.1572-0241.1999.01377.x.
Ratziu V, Charlotte F, Heurtier A, Gombert S, Giral P, Bruckert E, et al. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology 2005;128:1898-1906. https://doi.org/10.1053/j.gastro.2005.03.084.
Cobo-Martín M, Fernández Gil P, Crespo J. [Treatment of fatty liver disease]. Gastroenterol Hepatol 2008;31:229-238. https://doi.org/10.1157/13117902.
Carlsson LM, Peltonen M, Ahlin S, Anveden Å, Bouchard C, Carlsson B, et al. Bariatric surgery and prevention of type 2 diabetes in Swedish obese subjects. N Engl J Med 2012;367:695-704. https://doi.org/10.1056/NEJMoa1112082.
Kaser S, Ebenbichler CF, Tilg H. Pharmacological and non-pharmacological treatment of non-alcoholic fatty liver disease. Int J Clin Pract 2010;64:968-983. https://doi.org/10.1111/j.1742-1241.2009.02327.x.
Liss KH, Finck BN. PPARs and nonalcoholic fatty liver disease. Biochimie 2017;136:65-74. https://doi.org/10.1016/j.biochi.2016.11.009.
Musso G, Gambino R, Cassader M, Pagano G. A meta-analysis of randomized trials for the treatment of nonalcoholic fatty liver disease. Hepatology 2010;52:79-104. https://doi.org/10.1002/hep.23623.
Sanyal AJ, Chalasani N, Kowdley KV, McCullough A, Diehl AM, Bass NM, et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med 2010;362:1675-1685. https://doi.org/10.1056/NEJMoa0907929.
Pop LM, Lingvay I, Yuan Q, Li X, Adams-Huet B, Maalouf NM. Impact of pioglitazone on bone mineral density and bone marrow fat content. Osteoporos Int 2017;28:3261-3269. https://doi.org/10.1007/s00198-017-4164-3.
Singh S, Khera R, Allen AM, Murad MH, Loomba R. Comparative effectiveness of pharmacological interventions for nonalcoholic steatohepatitis: A systematic review and network meta-analysis. Hepatology 2015;62:1417-1432. https://doi.org/10.1002/hep.27999.
Schürks M, Glynn RJ, Rist PM, Tzourio C, Kurth T. Effects of vitamin E on stroke subtypes: meta-analysis of randomised controlled trials. Bmj 2010;341:c5702. https://doi.org/10.1136/bmj.c5702.
Wyatt G. Vitamin E increases prostate cancer risk in middle-aged men relative to placebo: no significant association observed with selenium, either alone or in combination with vitamin E. Evid Based Nurs 2012;15:90-91. https://doi.org/10.1136/ebnurs-2012-100551.
Thondam SK, Cuthbertson DJ, Aditya BS, Macfarlane IA, Wilding JP, Daousi C. A glucagon-like peptide-1 (GLP-1) receptor agonist in the treatment for hypothalamic obesity complicated by type 2 diabetes mellitus. Clin Endocrinol (Oxf) 2012;77:635-637. https://doi.org/10.1111/j.1365-2265.2012.04368.x.
Cuthbertson DJ, Irwin A, Gardner CJ, Daousi C, Purewal T, Furlong N, et al. Improved glycaemia correlates with liver fat reduction in obese, type 2 diabetes, patients given glucagon-like peptide-1 (GLP-1) receptor agonists. PloS one 2012;7:e50117. https://doi.org/10.1371/journal.pone.0050117.
Armstrong MJ, Gaunt P, Aithal GP, Barton D, Hull D, Parker R, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet 2016;387:679-690. https://doi.org/10.1016/s0140-6736(15)00803-x.
Newsome PN, Buchholtz K, Cusi K, Linder M, Okanoue T, Ratziu V, et al. A placebo-controlled trial of subcutaneous semaglutide in nonalcoholic steatohepatitis. N Engl J Med 2021;384:1113-1124. https://doi.org/10.1056/NEJMoa2028395.
Adorini L, Pruzanski M, Shapiro D. Farnesoid X receptor targeting to treat nonalcoholic steatohepatitis. Drug Discov Today 2012;17:988-997. https://doi.org/10.1016/j.drudis.2012.05.012.
Neuschwander-Tetri BA, Loomba R, Sanyal AJ, Lavine JE, Van Natta ML, Abdelmalek MF, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial. Lancet 2015;385:956-965. https://doi.org/10.1016/s0140-6736(14)61933-4.
Younossi ZM, Ratziu V, Loomba R, Rinella M, Anstee QM, Goodman Z, et al. Obeticholic acid for the treatment of non-alcoholic steatohepatitis: interim analysis from a multicentre, randomised, placebo-controlled phase 3 trial. Lancet 2019;394:2184-2196. https://doi.org/10.1016/s0140-6736(19)33041-7.
Rakoski MO, Singal AG, Rogers MA, Conjeevaram H. Meta-analysis: insulin sensitizers for the treatment of non-alcoholic steatohepatitis. Aliment Pharmacol Ther 2010;32:1211-1221. https://doi.org/10.1111/j.1365-2036.2010.04467.x.
Singh S, Singh PP, Roberts LR, Sanchez W. Chemopreventive strategies in hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol 2014;11:45-54. https://doi.org/10.1038/nrgastro.2013.143.
Leuschner UF, Lindenthal B, Herrmann G, Arnold JC, Rössle M, Cordes HJ, et al. High-dose ursodeoxycholic acid therapy for nonalcoholic steatohepatitis: a double-blind, randomized, placebo-controlled trial. Hepatology 2010;52:472-479. https://doi.org/10.1002/hep.23727.
Lindor KD, Kowdley KV, Heathcote EJ, Harrison ME, Jorgensen R, Angulo P, et al. Ursodeoxycholic acid for treatment of nonalcoholic steatohepatitis: results of a randomized trial. Hepatology 2004;39:770-778. https://doi.org/10.1002/hep.20092.
Descargas
Publicado
Cómo citar
Número
Sección
Licencia

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
La política de reconocimiento de autoría de Hepatología se basa en los criterios indicados por el ICMJE para conferir crédito de un trabajo a una persona, a la vez que se le atribuye responsabilidad por la publicación del mismo.