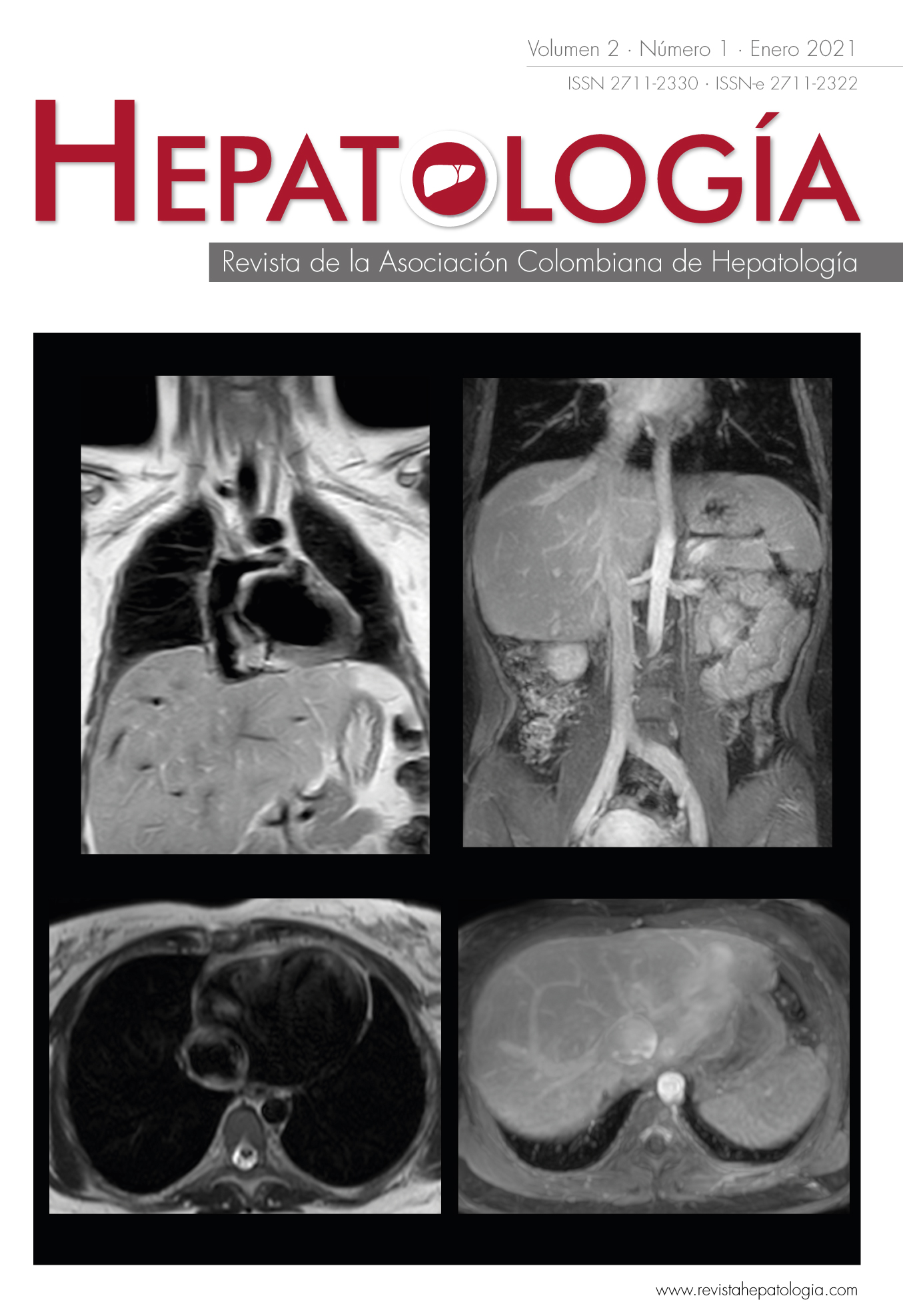
Fontan-associated liver disease: report of two cases and literature review
DOI:
https://doi.org/10.52784/27112330.131Keywords:
Fontan procedure, univentricular heart, liver cirrhosis, liver diseases, hepatocellular carcinoma.Abstract
Fontan surgery diverts the flow of the inferior vena cava through a cavopulmonary anastomosis, to avoid mixing the oxygenated and non-oxygenated blood, in the presence of tricuspid atresia associated with hypoplastic ventricle. The physiological changes produced by this new circulation have several consequences at cardiac and extracardiac level, including the liver, with multiple descriptions of chronic liver disease of vascular origin, and even hepatocellular carcinoma in cirrhotic liver at an early age. With the aim of a better understanding of liver complications caused by this procedure, two clinical cases are described and a literature review is presented. Despite the fact that Fontan-associated liver disease is a rare entity, hepatologists must keep it in mind and learn how to recognize it, since an adequate follow-up can make the difference when effectively selecting those patients who would benefit from a single or combined liver and/or heart transplant, as well as allowing the early detection of devastating complications such as advanced stage hepatocellular carcinoma.
Downloads
References
Fontan F, Baudet E. Surgical repair of tricuspid atresia. Thorax 1971;26:240-248. https://doi.org/10.1136/thx.26.3.240.
de Leval MR, Deanfield JE. Four decades of Fontan palliation. Nat Rev Cardiol 2010;7:520-527. https://doi.org/10.1038/nrcardio.2010.99.
Oh C, Youn JK, Han J-W, Kim GB, Kim H-Y, Jung S-E. Hepatocellular carcinoma after the Fontan procedure in a 16-year-old girl: A case report. Medicine 2016;95:e4823. https://doi.org/10.1097/MD.0000000000004823.
Egbe AC, Poterucha JT, Warnes CA, Connolly HM, Baskar S, Ginde S, et al. Hepatocellular carcinoma after Fontan operation. Circulation 2018;138:746-748. https://doi.org/doi:10.1161/CIRCULATIONAHA.117.032717.
Kuwabara M, Niwa K, Toyoda T, Shirai T, Tateno S, Ohuchi H, et al. Liver cirrhosis and/or hepatocellular carcinoma occurring late after the Fontan procedure-A nationwide survey in Japan. Circ J 2018;82:1155-1160. https://doi.org/10.1253/circj.CJ-17-1053.
Gewillig M, Brown SC. The Fontan circulation after 45 years: update in physiology. Heart 2016;102:1081-1086. https://doi.org/10.1136/heartjnl-2015-307467.
Kalfa D. Fontan-associated liver disease: Is it all about hemodynamics? J Thorac Cardiovasc Surg 2018;156:276-277. https://doi.org/10.1016/j.jtcvs.2018.03.104.
Rathgeber SL, Harris KC. Fontan-associated liver disease: Evidence for early surveillance of liver health in pediatric Fontan patients. Can J Cardiol 2019;35:217-220. https://doi.org/10.1016/j.cjca.2018.11.019.
Schwartz MC, Sullivan L, Cohen MS, Russo P, John AS, Guo R, et al. Hepatic pathology may develop before the Fontan operation in children with functional single ventricle: an autopsy study. J Thorac Cardiovasc Surg 2012;143:904-909. https://doi.org/10.1016/j.jtcvs.2011.08.038.
Baek JS, Bae EJ, Ko JS, Kim GB, Kwon BS, Lee SY, et al. Late hepatic complications after Fontan operation; non-invasive markers of hepatic fibrosis and risk factors. Heart 2010;96:1750-1755. https://doi.org/10.1136/hrt.2010.201772.
Ackerman T, Geerts A, Van Vlierberghe H, De Backer J, François K. Hepatic changes in the Fontan circulation: Identification of liver dysfunction and an attempt to streamline follow-up screening. Pediatr Cardiol 2018;39:1604-1613. https://doi.org/10.1007/s00246-018-1937-1.
Téllez L, Rodríguez-Santiago E, Albillos A. Fontan-associated liver disease: A review. Ann Hepatol 2018;17:192-204. https://doi.org/https://doi.org/10.5604/01.3001.0010.8634.
Song J, Kim K, Huh J, Kang IS, Kim SH, Yang JH, et al. Imaging assessment of hepatic changes after Fontan surgery. Int Heart J 2018;59:1008-1014. https://doi.org/10.1536/ihj.17-349.
Ho SSK, Brown R, Fitzgibbon B. Hepatocellular carcinoma with cardiac cirrhosis. Med J Aust 1990;152:553-554. https://doi.org/10.5694/j.1326-5377.1990.tb125362.x.
Wells ML, Hough DM, Fidler JL, Kamath PS, Poterucha JT, Venkatesh SK. Benign nodules in post-Fontan livers can show imaging features considered diagnostic for hepatocellular carcinoma. Abdom Radiol 2017;42:2623-2631. https://doi.org/10.1007/s00261-017-1181-9.
Horvat N, Rocha MS, Chagas AL, Oliveira BC, Pacheco MP, Binotto MA, et al. Multimodality screening of hepatic nodules in patients with congenital heart disease after Fontan procedure: Role of ultrasound, ARFI elastography, CT, and MRI. Am J Roentgenol 2018;211:1212-1220. https://doi.org/10.2214/AJR.18.19762.
Rathgeber SL, Guttman OR, Lee AF, Voss C, Hemphill NM, Schreiber RA, et al. Fontan-associated liver disease: Spectrum of disease in children and adolescents. J Am Heart Assoc 2020;9:e012529. https://doi.org/10.1161/jaha.119.012529.
Emamaullee J, Zaidi AN, Schiano T, Kahn J, Valentino PL, Hofer RE, et al. Fontan-associated liver disease. Circulation 2020;142:591-604. https://doi.org/doi:10.1161/CIRCULATIONAHA.120.045597.
Simpson KE, Esmaeeli A, Khanna G, White F, Turnmelle Y, Eghtesady P, et al. Liver cirrhosis in Fontan patients does not affect 1-year post-heart transplant mortality or markers of liver function. J Heart Lung Transplant 2014;33:170-177. https://doi.org/10.1016/j.healun.2013.10.033.
Cannon RM, Hughes MG, Jones CM, Eng M, Marvin MR. A review of the United States experience with combined heart-liver transplantation. Transpl Int 2012;25:1223-1228. https://doi.org/10.1111/j.1432-2277.2012.01551.x.
Hilscher MB, Johnson JN, Cetta F, Driscoll DJ, Poterucha JJ, Sanchez W, et al. Surveillance for liver complications after the Fontan procedure. Congenit Heart Dis 2017;12:124-132. https://doi.org/10.1111/chd.12446.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
La política de reconocimiento de autoría de Hepatología se basa en los criterios indicados por el ICMJE para conferir crédito de un trabajo a una persona, a la vez que se le atribuye responsabilidad por la publicación del mismo.