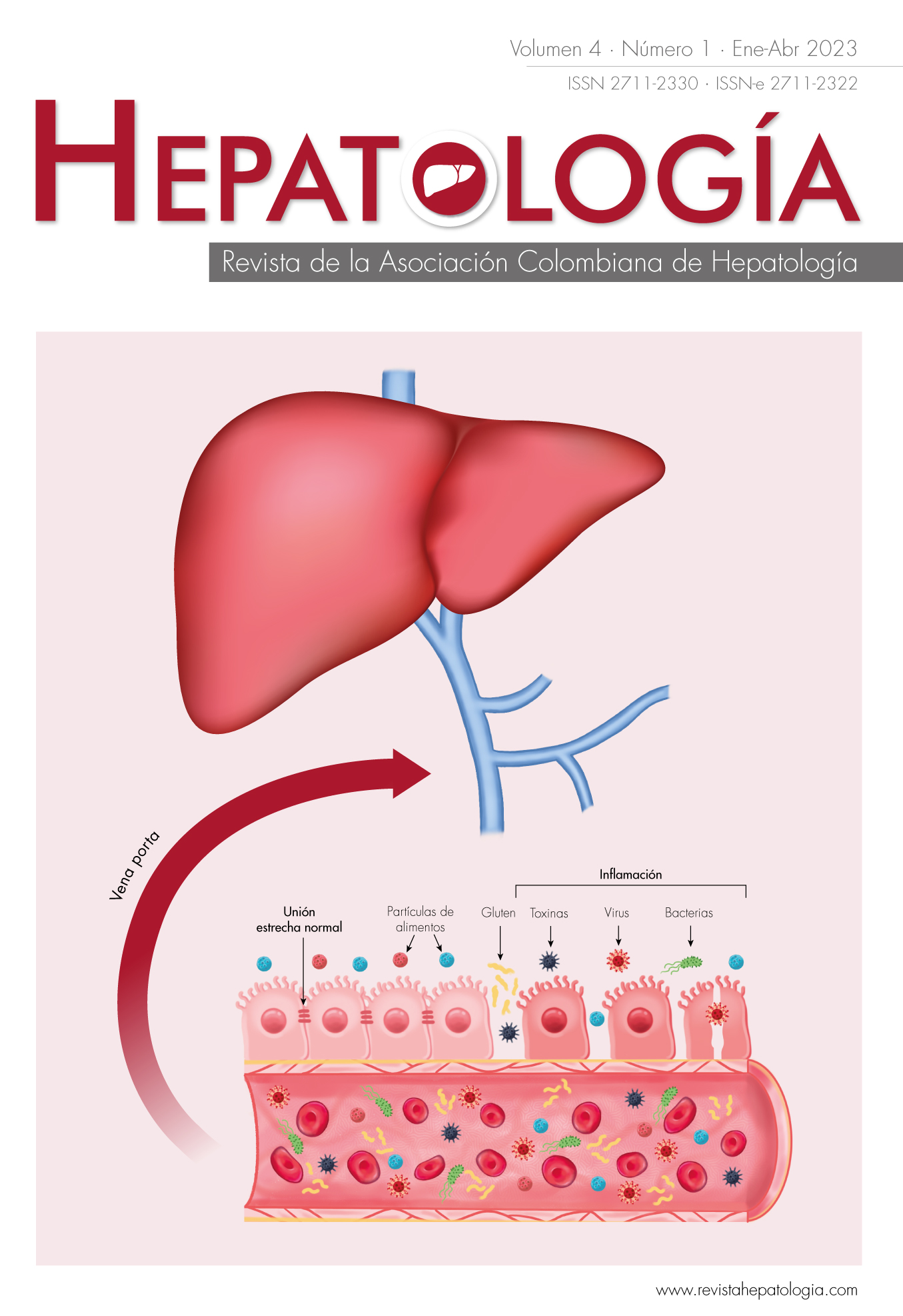
Alteración de la microbiota intestinal y su relación con enfermedades gastrointestinales y hepatobiliares
DOI:
https://doi.org/10.52784/27112330.168Palabras clave:
microbioma, microbiota, Bacteroidetes, Firmicutes, Proteobacterias, factores de riesgo, disbiosis, enfermedades gastrointestinales, trastornos hepatobiliares, prebióticos, probióticos.Resumen
La interrupción de la simbiosis que existe entre el cuerpo humano y su microbioma puede resultar en una disbiosis, un desequilibrio en la interacción huésped-microbiota, que puede asociarse al desarrollo de diversas enfermedades como el síndrome de intestino irritable, hígado graso no alcohólico, enfermedad hepática alcohólica y cirrosis, entre otras. En ciertas condiciones patológicas y por múltiples factores de riesgo, la capacidad de autorregulación del intestino se puede alterar, contribuyendo al incremento de la permeabilidad con inflamación intestinal crónica. El diagnóstico y el tratamiento, así como la relación entre la permeabilidad intestinal, la disbiosis y las patologías gastrointestinales y hepatobiliares, todavía no tienen estudios clínicos validados o con el soporte científico adecuado, por lo que se realiza una revisión de la literatura con la finalidad de aportar conceptos que puedan orientar con respecto a la importancia del estudio del microbioma humano en estas enfermedades.
Descargas
Referencias bibliográficas
Konturek PC, Harsch IA, Konturek K, Schink M, Konturek T, Neurath MF, et al. Gut⁻liver axis: How do gut bacteria influence the liver? Med Sci (Basel) 2018;6:79. https://doi.org/10.3390/medsci6030079.
Andreola F, Moliterni C, Quagliariello A, Scaldaferri F, Fidaleo M. Editorial: The role of microbiota in the onset and development of intestine and liver diseases and cancer: Molecular and cell mechanisms. Front Cell Dev Biol 2022;10:852188. https://doi.org/10.3389/fcell.2022.852188.
Gomaa EZ. Human gut microbiota/microbiome in health and diseases: a review. Antonie Van Leeuwenhoek 2020;113:2019-2040. https://doi.org/10.1007/s10482-020-01474-7.
Ding JH, Jin Z, Yang XX, Lou J, Shan WX, Hu YX, et al. Role of gut microbiota via the gut-liver-brain axis in digestive diseases. World J Gastroenterol 2020;26:6141-6162. https://doi.org/10.3748/wjg.v26.i40.6141.
Gómez-Eguílaz M, Ramón-Trapero JL, Pérez-Martínez L, Blanco JR. El eje microbiota-intestino-cerebro y sus grandes proyecciones. Rev Neurol 2019;68:0111-0117. https://doi.org/10.33588/rn.6803.2018223.
Agudelo-Ochoa GM, Giraldo-Giraldo NA, Barrera-Causil CJ, Valdés-Duque BE. Microbiota intestinal y ácidos grasos de cadena corta en pacientes críticos. Perspect Nutr Hum 2016;18:205-222.
Chopyk DM, Grakoui A. Contribution of the intestinal microbiome and gut barrier to hepatic disorders. Gastroenterology 2020;159:849-863. https://doi.org/10.1053/j.gastro.2020.04.077.
Fukui H. Role of gut dysbiosis in liver diseases: What have we learned so far? Diseases 2019;7:58. https://doi.org/10.3390/diseases7040058.
Gupta H, Youn GS, Shin MJ, Suk KT. Role of gut microbiota in hepatocarcinogenesis. Microorganisms 2019;7:121. https://doi.org/10.3390/microorganisms7050121.
Salles-Teixeira TF, Boroni-Moreira AP, Silva-Souza NC, Frias R, Gouveia-Peluzio Mdo C. Intestinal permeability measurements: general aspects and possible pitfalls. Nutr Hosp 2014;29:269-281. https://doi.org/10.3305/nh.2014.29.2.7076.
Vancamelbeke M, Vermeire S. The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol 2017;11:821-834. https://doi.org/10.1080/17474124.2017.1343143.
Monda V, Villano I, Messina A, Valenzano A, Esposito T, Moscatelli F, et al. Exercise modifies the gut microbiota with positive health effects. Oxid Med Cell Longev 2017;2017:3831972. https://doi.org/10.1155/2017/3831972.
Paray BA, Albeshr MF, Jan AT, Rather IA. Leaky gut and autoimmunity: An intricate balance in individuals health and the diseased state. Int J Mol Sci 2020;21:9770. https://doi.org/10.3390/ijms21249770.
Mamieva Z, Poluektova E, Svistushkin V, Sobolev V, Shifrin O, Guarner F, et al. Antibiotics, gut microbiota, and irritable bowel syndrome: What are the relations? World J Gastroenterol 2022;28:1204-1219. https://doi.org/10.3748/wjg.v28.i12.1204.
Aguirre-Valadez JM, Rivera-Espinosa L, Méndez-Guerrero O, Chávez-Pacheco JL, García-Juárez I, Torre A. Intestinal permeability in a patient with liver cirrhosis. Ther Clin Risk Manag 2016;12:1729-1748. https://doi.org/10.2147/tcrm.S115902.
Salvo-Romero E, Alonso-Cotoner C, Pardo-Camacho C, Casado-Bedmar M, Vicario M. The intestinal barrier function and its involvement in digestive disease. Rev Esp Enferm Dig 2015;107:686-696.
Camilleri M. Leaky gut: mechanisms, measurement and clinical implications in humans. Gut 2019;68:1516-1526. https://doi.org/10.1136/gutjnl-2019-318427.
Tran CD, Grice DM, Wade B, Kerr CA, Bauer DC, Li D, et al. Gut permeability, its interaction with gut microflora and effects on metabolic health are mediated by the lymphatics system, liver and bile acid. Future Microbiol 2015;10:1339-1353. https://doi.org/10.2217/fmb.15.54.
Kessoku T, Kobayashi T, Tanaka K, Yamamoto A, Takahashi K, Iwaki M, et al. The role of leaky gut in nonalcoholic fatty liver disease: A novel therapeutic target. Int J Mol Sci 2021;22. https://doi.org/10.3390/ijms22158161.
Nishimura N, Kaji K, Kitagawa K, Sawada Y, Furukawa M, Ozutsumi T, et al. Intestinal permeability is a mechanical rheostat in the pathogenesis of liver cirrhosis. Int J Mol Sci 2021;22:6921. https://doi.org/10.3390/ijms22136921.
Wang Y, Zhang Y, Liu Y, Xu J, Liu Y. Gut-liver axis: Liver sinusoidal endothelial cells function as the hepatic barrier in colitis-induced liver injury. Front Cell Dev Biol 2021;9:702890. https://doi.org/10.3389/fcell.2021.702890.
Campion D, Giovo I, Ponzo P, Saracco GM, Balzola F, Alessandria C. Dietary approach and gut microbiota modulation for chronic hepatic encephalopathy in cirrhosis. World J Hepatol 2019;11:489-512. https://doi.org/10.4254/wjh.v11.i6.489.
Patel VC, White H, Støy S, Bajaj JS, Shawcross DL. Clinical science workshop: targeting the gut-liver-brain axis. Metab Brain Dis 2016;31:1327-1337. https://doi.org/10.1007/s11011-015-9743-4.
Chen M, Ruan G, Chen L, Ying S, Li G, Xu F, et al. Neurotransmitter and intestinal interactions: Focus on the microbiota-gut-brain axis in irritable bowel syndrome. Front Endocrinol (Lausanne) 2022;13:817100. https://doi.org/10.3389/fendo.2022.817100.
Randulff-Hillestad EM, van der Meeren A, Nagaraja BH, Bjørsvik BR, Haleem N, Benitez-Paez A, et al. Gut bless you: The microbiota-gut-brain axis in irritable bowel syndrome. World J Gastroenterol 2022;28:412-431. https://doi.org/10.3748/wjg.v28.i4.412.
Ghaffari P, Shoaie S, Nielsen LK. Irritable bowel syndrome and microbiome; Switching from conventional diagnosis and therapies to personalized interventions. J Transl Med 2022;20:173. https://doi.org/10.1186/s12967-022-03365-z.
Hrncir T. Gut microbiota dysbiosis: Triggers, consequences, diagnostic and therapeutic options. Microorganisms 2022;10:578. https://doi.org/10.3390/microorganisms10030578.
Nishida A, Inoue R, Inatomi O, Bamba S, Naito Y, Andoh A. Gut microbiota in the pathogenesis of inflammatory bowel disease. Clin J Gastroenterol 2018;11:1-10. https://doi.org/10.1007/s12328-017-0813-5.
Schupack DA, Mars RAT, Voelker DH, Abeykoon JP, Kashyap PC. The promise of the gut microbiome as part of individualized treatment strategies. Nat Rev Gastroenterol Hepatol 2022;19:7-25. https://doi.org/10.1038/s41575-021-00499-1.
Ilan Y. Leaky gut and the liver: a role for bacterial translocation in nonalcoholic steatohepatitis. World J Gastroenterol 2012;18:2609-2618. https://doi.org/10.3748/wjg.v18.i21.2609.
Jiang D, Zhang J, Lin S, Wang Y, Chen Y, Fan J. Prolyl endopeptidase gene disruption improves gut dysbiosis and non-alcoholic fatty liver disease in mice induced by a high-fat diet. Front Cell Dev Biol 2021;9:628143. https://doi.org/10.3389/fcell.2021.628143.
Hartmann P, Chen WC, Schnabl B. The intestinal microbiome and the leaky gut as therapeutic targets in alcoholic liver disease. Front Physiol 2012;3:402. https://doi.org/10.3389/fphys.2012.00402.
Meroni M, Longo M, Dongiovanni P. Alcohol or gut microbiota: Who is the guilty? Int J Mol Sci 2019;20:4568. https://doi.org/10.3390/ijms20184568.
Méndez-Sánchez N, Valencia-Rodriguez A, Vera-Barajas A, Abenavoli L, Scarpellini E, Ponciano-Rodriguez G, et al. The mechanism of dysbiosis in alcoholic liver disease leading to liver cancer. Hepatoma Res 2020;6:5. https://doi.org/10.20517/2394-5079.2019.29.
Fukui H. Leaky gut and gut-liver axis in liver cirrhosis: Clinical studies update. Gut Liver 2021;15:666-676. https://doi.org/10.5009/gnl20032.
Mancini A, Campagna F, Amodio P, Tuohy KM. Gut : liver : brain axis: the microbial challenge in the hepatic encephalopathy. Food Funct 2018;9:1373-1388. https://doi.org/10.1039/c7fo01528c.
Yu LX, Schwabe RF. The gut microbiome and liver cancer: mechanisms and clinical translation. Nat Rev Gastroenterol Hepatol 2017;14:527-539. https://doi.org/10.1038/nrgastro.2017.72.
Wang L, Llorente C, Hartmann P, Yang AM, Chen P, Schnabl B. Methods to determine intestinal permeability and bacterial translocation during liver disease. J Immunol Methods 2015;421:44-53. https://doi.org/10.1016/j.jim.2014.12.015.
Usuda H, Okamoto T, Wada K. Leaky gut: Effect of dietary fiber and fats on microbiome and intestinal barrier. Int J Mol Sci 2021;22:7613. https://doi.org/10.3390/ijms22147613.
Matsuda K, Tsuji H, Asahara T, Matsumoto K, Takada T, Nomoto K. Establishment of an Analytical System for the Human Fecal Microbiota, Based on Reverse Transcription-Quantitative PCR Targeting of Multicopy rRNA Molecules. J Appl Environ Microbiol 2009;75:1961-1969. https://doi.org/doi:10.1128/AEM.01843-08.
Haakensen M, Dobson CM, Deneer H, Ziola B. Real-time PCR detection of bacteria belonging to the Firmicutes Phylum. Int J Food Microbiol 2008;125:236-241. https://doi.org/10.1016/j.ijfoodmicro.2008.04.002.
Jo YJ, Tagele SB, Pham HQ, Jung Y, Ibal JC, Choi S, et al. In situ profiling of the three dominant phyla within the human gut using TaqMan PCR for pre-hospital diagnosis of gut dysbiosis. Int J Mol Sci 2020;21:1916. https://doi.org/10.3390/ijms21061916.
Sharon G, Garg N, Debelius J, Knight R, Dorrestein Pieter C, Mazmanian Sarkis K. Specialized metabolites from the microbiome in health and disease. Cell Metab 2014;20:719-730. https://doi.org/10.1016/j.cmet.2014.10.016.
Shah A, Talley NJ, Holtmann G. Current and future approaches for diagnosing small intestinal dysbiosis in patients with symptoms of functional dyspepsia. Front Neurosci 2022;16:830356. https://doi.org/10.3389/fnins.2022.830356.
Maslennikov R, Ivashkin V, Efremova I, Poluektova E, Kudryavtseva A, Krasnov G. Gut dysbiosis and small intestinal bacterial overgrowth as independent forms of gut microbiota disorders in cirrhosis. World J Gastroenterol 2022;28:1067-1077. https://doi.org/10.3748/wjg.v28.i10.1067.
Koch M. Gut microbiota and the liver: A tale of 2 cities: A narrative view in 2 acts. J Clin Gastroenterol 2016;50:S183-s187. https://doi.org/10.1097/mcg.0000000000000699.
Paolella G, Mandato C, Pierri L, Poeta M, Di Stasi M, Vajro P. Gut-liver axis and probiotics: their role in non-alcoholic fatty liver disease. World J Gastroenterol 2014;20:15518-15531. https://doi.org/10.3748/wjg.v20.i42.15518.
Song Q, Zhang X. The role of gut-liver axis in gut microbiome dysbiosis associated NAFLD and NAFLD-HCC. Biomedicines 2022;10:524. https://doi.org/10.3390/biomedicines10030524.
Schnabl B. Linking intestinal homeostasis and liver disease. Curr Opin Gastroenterol 2013;29:264-270. https://doi.org/10.1097/MOG.0b013e32835ff948.
Limas-Solano LM, Vargas-Niño CE, Valbuena-Rodríguez DC, Ramírez-López LX. Trasplante de microbiota fecal: una revisión. Rev Col Gastroenterol 2020;35:329-337. https://doi.org/10.22516/25007440.486.
U.S. Food and Drug Administration (FDA). Important safety alert regarding use of fecal microbiota for transplantation and risk of serious adverse reactions due to transmission of multi-drug resistant organisms. Maryland, Estados Unidos: FDA; 2019. Acceso 5 de septiembre de 2022. Disponible en https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/important-safety-alert-regarding-use-fecal-microbiota-transplantation-and-risk-serious-adverse.
Chang L, Wei Y, Hashimoto K. Brain-gut-microbiota axis in depression: A historical overview and future directions. Brain Res Bull 2022;182:44-56. https://doi.org/10.1016/j.brainresbull.2022.02.004.
Al-Ayadhi L, Zayed N, Bhat RS, Moubayed NMS, Al-Muammar MN, El-Ansary A. The use of biomarkers associated with leaky gut as a diagnostic tool for early intervention in autism spectrum disorder: a systematic review. Gut Pathog 2021;13:54. https://doi.org/10.1186/s13099-021-00448-y.
Real-López M, Peraire M, Ramos-Vidal C, Nath D, Hervás A, X. C. Implicación de la disbiosis intestinal en la etiopatogenia y el tratamiento del trastorno del espectro autista: una revisión bibliográfica. Rev Neurol 2021;73:282-295.
Yeoh YK, Zuo T, Lui GC-Y, Zhang F, Liu Q, Li AY, et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut 2021;70:698-706. https://doi.org/10.1136/gutjnl-2020-323020.
Farsi Y, Tahvildari A, Arbabi M, Vazife F, Sechi LA, Shahidi Bonjar AH, et al. Diagnostic, prognostic, and therapeutic roles of gut microbiota in COVID-19: A comprehensive systematic review. Front Cell Infect Microbiol 2022;12:804644. https://doi.org/10.3389/fcimb.2022.804644.
Descargas
Publicado
Cómo citar
Número
Sección
Licencia

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
La política de reconocimiento de autoría de Hepatología se basa en los criterios indicados por el ICMJE para conferir crédito de un trabajo a una persona, a la vez que se le atribuye responsabilidad por la publicación del mismo.